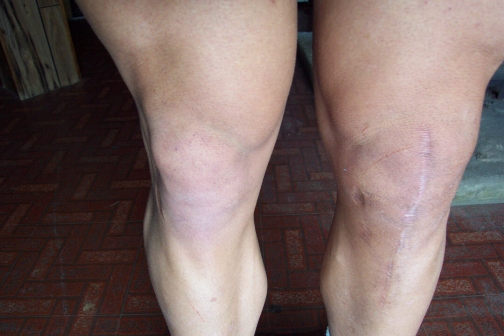
Comparison of both knees - 14 months post-ACI


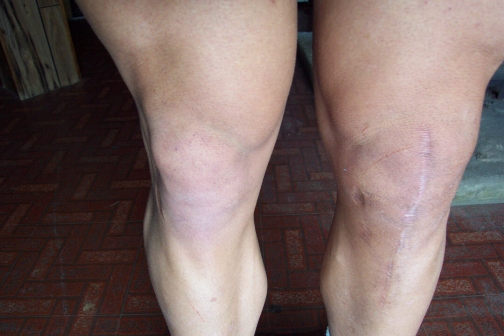
Images of left knee - 14 months post-ACI
The surgery is scheduled for 8:00 AM and things go as planned. I leave the surgical center by 12:30 PM with a collection of new sensations brought on by the combination of anesthesia, pain medication, and the trauma of the surgery itself.
December 28 - afternoon of surgeryThe procedure is more involved than anything I've had before, so I expect things to be a little more painful than with the ACL reconstructions. The pain medications are effective for most of the day, so I'm mainly just uncomfortable and inconvenienced. To the best of my recollection, the sensations are similar to what I felt after the ACL reconstructions. The effects of the anesthesia are worse than the knee pain and I mainly sleep away the afternoon and early evening.
December 28 - night of surgery
OK, the pain medication given at the surgical center has well worn-off by now and I sure notice it. However, it's not excruciatingly painful and I didn't use pain medication in any of my previous surgeries so I plan to stick this out. At roughly 5 AM, I give in. I've not slept much at all and it's impossible to find a comfortable position so I take a few Percocets and fall asleep shortly thereafter.
A member of the surgeon's staff changes the dressings. I expect things to appear worse than I'd seen in my earlier procedures and this is the case. There is absolutely no trace of a knee as I know it. The swelling is much greater and there's more bruising than in any of the previous operations. The wound is closed on the surface by about 30 staples. The surgeon tells me that things went OK and that the lesions I had were larger than average (medial femoral condyle lesion - 8.75 cm2 and lateral femoral condyle lesion - 5.5 cm2) but we knew this already from the biopsy performed a month ago. Based on the earlier biopsy and the damage assessment performed at that time, Genzyme cultured over twice the number (20 million) of cells that are generated under average conditions (5 to 10 million). My surgeon tells me he injected everything they sent which was probably more than needed. I asked the obvious question - "Do you realize any acceleration in the process if you start with more cells at the beginning?" Unfortunately, the answer is no. I'm also encouraged to increase the range of flexion on the CPM machine whenever I feel comfortable doing so.
Week One - General Notes
The remainder of the week is largely uneventful, I'm in the continuous passive motion (CPM), along with the Polar Care cryotherapy, machines for about eight hours a day and all of my remaining time is spent doing the most basic things you need to get through the day. I've progressed from 30 degrees flexion to about 40 degrees but feel like I could extend this range easily. The immobilizing brace is on for the entire week, whenever I'm not in the CPM machine. I probably average between 7.5 to 8 hours, daily, in the CPM machine. I take the pain medicine twice per day, mainly to help sleep. The worst pain comes with standing after lying down, blood rushes to the knee and brings waves of sharp sensations. It takes a few seconds to adjust and then it's tolerable. On Friday, January 1, I drive to the local bank and the grocery store both of which are close to home - challenging and uncomfortable.
I drive to the surgeon's office for my second post-op visit. This is inconvenient and the 15-minute drive is about the limit but things work out OK. The staples are removed and I get the OK to start therapy on the following Monday. The swelling is still substantial but doesn't merit having the knee drained.
January 7 - post-op visit #3I notice that the wound is oozing a bit from the middle of the larger incision. I clean it up and call the surgeon's office as the gap in the wound seems wide and I wonder if it might need another set of stitches or staples. My surgeon requests that I come in for a quick look; the wound is cleaned and a surface culture is taken from the wound. The doctor also suggests draining the knee with the hope of withdrawing fluid to have examined for signs of bacterial infection. A small amount of fluid is taken from within the knee but only after a several attempts; this indicates that most of the swelling lies within the soft tissue of the knee. I take the surface culture, and the fluid taken by aspiration, to a hospital pathology lab for tests. Physical therapy, that had been scheduled for the following Monday, January 10 is delayed until the lab test results are in.
January 8The day after my unscheduled third visit to the surgeon I feel OK. The swelling hasn't increased and I don't have a fever so I feel pretty good about there being no infection. I'm able to comfortably extend the flexion setting on the CPM machine to about 60 degrees.
January 9Not exactly earth-shattering but the wound has closed and I feel pretty confident in taking my first post-op shower. I've done this before, following previous ACL reconstructions, but the challenge of getting in and out of a tub, as well as showering while using only one leg, must be tried to be fully appreciated.
Week Two - General NotesAside from the events described above, the second week is similar to the first. I'm still in the CPM machine for nearly 8 hours per day.
My second shower doesn't go as smoothly as the first. Getting out of the tub, I fall. Most of my weight is absorbed by my good (right) leg and my left elbow. The bad leg does extend and hits the back of the tub in full extension. So, it does take some shock though not nearly a full blow. This is very unsettling. My main fear has been a fall that directs force to the femoral condyles and, consequently, ruptures the periosteal patches holding in the cultured chondrocytes. But, I have no way of gauging whether my fall was enough to do so. I don't notice an increase in swelling after the fall. On a better note, I discover that the lab results indicate no infection; that's good news. RECOMMENDATION: use a plastic chair while showering during these first few weeks of instability.
January 12 - physical therapy session #1I'm the first ACI patient my therapist has seen but my surgeon has provided a copy of the rehabilitation protocol. In researching ACI, I've found a few copies of this protocol scattered across the web. I suppose since ACI is relatively new, everyone is more or less using the same protocol, a copy of which can be found at The Center for Orthopaedics and Sports Medicine (Marietta, GA) web site, in the section: ACI rehabilitation protocols. The therapist notes that the swelling is well above average compared to that seen with other knee surgery (ACL, menisectomy, etc.) patients at this stage. This isn't unexpected since most knee surgeries are less invasive. The ACI procedure is performed in an arthrotomy and is quite traumatic by comparison with ACL reconstructions and menisectomies, both of which are arthroscopic procedures. The therapist performs an assessment (range of motion, lag, and contraction of the vastus medialis oblique) and electrical stimulation is applied to assist with quadricep contraction. Other than that, the activities I'm able to perform are very limited - straight leg raises and heel slides. I'll start to do these on my own at home as well as in therapy visits.
January 13 - post-op visit #4My visit to the surgeon is fairly uneventful. I tell him that I'm at 75 degrees flexion on the CPM machine and I'm told that I'll no longer need the machine after I've reached 90 degrees. I ask about my fall earlier in the week and my surgeon doesn't seem too alarmed. He said the real concern would be a full weight-bearing fall that involved twisting; the implantation site is most vulnerable to shearing forces. However, he said there's no sure technique, aside from surgery, to assess any damage that may have occurred.
January 14 - physical therapy session #2The routine is the same as the first day of therapy. In reviewing the protocol with my therapist, we note a discrepancy between what is specified there (partial weight-bearing at 2-4 weeks) and what I've been told directly (no weight-bearing for at least 6 weeks). This is to be discussed with the surgeon. Apparently, it's a bad week for falling. My crutches slip off of a step and I hit the involved leg on the step below. It's a fairly quick event and I catch myself with the crutches before my full weight is absorbed. Again, I have no idea what may have been done but my knee doesn't show outward signs of any further damage.
January 17 - physical therapy session #3My therapist hasn't yet heard from the surgeon regarding the differences among my directions and the protocol specifications. It's decided to play things conservatively (no weight-bearing). I begin stationary bike exercises with no resistance. This consists mainly of pendulum-type movements as I don't have the range of motion to complete a full revolution. Multi-hip machine exercises take the place of straight leg raises but there are no significant changes otherwise. Without weight-bearing status, the limitations are significant and there's little that I do in the formal setting of physical therapy that I can't do at home. In addition to this, there is the issue of insurance. My insurance company has agreed to pay for twelve visits. It's usually not difficult to convince an insurance company to pay for additional visits if they are justified. Nonetheless, there's still the risk given the ACI procedure isn't yet well-understood by insurance providers. Given these considerations, my therapist and I decide that two visits per week is adequate until I'm weight-bearing.
Week Three - General NotesI perform my home routine (heel slides, straight leg raises, isometric quadricep sets) roughly four times per day. I've advanced to 105 degrees flexion on the CPM machine but I decide to stay with it for a few more days. I've reduced time in the CPM machine from eight to roughly five hours each day. Since the wound has closed, I now feel comfortable applying emu oil to the incision. Emu oil, like Vitamin E, has anti-scarring properties. I've used both after previous surgeries and believe that emu oil is a bit more effective. In addition, emu oil is also reported to be an anti-inflammatory although I've not noticed any dramatic results in this area. From this point on, I apply emu oil to the wound roughly twice per day.
Nothing much changes in the routine from the previous visit. I'm at 115 degrees flexion and decide this is the last day of CPM machine use.
January 24 - physical therapy session #5Isometric leg extensions and leg curls are added to the routine. This involves adjusting the angle on the extension and curl machine but applying a "brake" so that no motion can occur. The swelling hasn't decreased noticeably for about a week or so but I'm still making gains in terms of flexion. I try massage the joint vigorously at home to reduce the swelling. This seems to work - the results aren't dramatic but noticeable, particularly beneath the patella.
Week Four - General NotesThe home routine remains the same. The knee is stiff in the morning but loosens quickly after a few heel slides and isometric quad sets. Early in the week, I begin to notice a pinching sensation in the area where the medial femoral condyle intersects the patella. I experienced the very same thing after my last ACL surgery. This was very limiting in the rehabilitation after that surgery as the pain was so sharp my therapist wouldn't allow me to work through some of the movements. After three weeks or so the pain gradually diminished until it was gone, indicative of scar tissue.
The routine is much the same as in the past few visits. I'm now able to complete full, not-so-smooth, revolutions on the stationary bike, still with no resistance though. The therapist performs and assessment and generates a report that I'll deliver to my surgeon tomorrow. In short, the swelling has decreased considerably beneath the patella but there isn't much change in the upper knee. Flexion is good - 114 degrees at the end of week four. I'm about a week ahead of the schedule given in the protocol (110 degrees at the end of week five). My therapist decides to try a pump for swelling reduction. After 15 minutes, the swelling has decreased 1.5 cm. It's difficult to determine whether this is mainly due to the pump, elevation, or ice.
January 27 - post-op visit #5My surgeon says that the knee looks good; the swelling and the associated warmth are more likely signs of healing as opposed to indicative of a problem. I ask about the discrepancy between the rehabilitation protocol and the direct, "no weight-bearing" instructions he gave me. He told me that the protocol is largely a living document and was developed with a single lesion in mind. Since I have two, my restrictions are a bit tighter. I also ask about the pinching sensation and remind the surgeon that the problem was present following the last ACL reconstruction. Assuming the problem is again scar tissue, I ask if I should push through it - the answer is yes but carefully. The area where I experience the pain is the spot of greatest deterioration. With regard to the short-term future, the current plan is to remain completely non weight-bearing until the five week mark. At five weeks, I'll begin toe-touching and very slight weight-bearing. Beginning at the sixth week, I'll walk for a few days with a cane or something similar until I'm confident with my balance.
January 28 - first visit to the gymI decide to go to the gym so that I'm able to use the stationary bike. I limit my time on the bike to 10 minutes. I repeat the routine I undergo during my regular physical therapy visits. I'm lucky since the gym has many of the same machines that are used at the therapy center. At home, I perform mainly mobilization exercises and, in addition, work on breaking up the scar tissue responsible for the pinching sensation described earlier.
January 29 - second visit to the gymI go to the gym again mainly to use the stationary bike. I'm a bit sore from yesterday but complete the routine again. Afterward I'm really sore, particularly behind the knee and in the area of the troublesome scar tissue.
General Notes - Week FiveThe consecutive days at the gym turn out to have been a bad idea. The joint, not the surrounding muscles, are too sore to think about doing much else other than mobilization movements. Lesson learned.
Surgery was five weeks ago, today marks the beginning of the sixth week post-op. It seems the swelling has decreased a bit but, as usual, the knee is stiff in the morning. After my home routine, I massage the knee for a while. I can feel scar tissue/adhesions/clots break apart as I apply firm pressure to the swollen areas above the knee. My knee is still sore but is better than the past two days. This is the week I begin toe-touching to reacquaint my feet with the ground.
February 2 - physical therapy session #7Things are still sore but I'm able to complete the regular routine without much difficulty. Seated hamstring curls are added to the routine. Afterward, I still have the pinching sensation and soreness behind the knee. In performing assisted prone leg curls (using my good leg to help), I notice that I don't experience the pinching sensation. As soon as I attempt to do these movement without assistance, the pain returns. More careful observation reveals that at the point of pain (on the medial side), I hit a scar tissue barrier (the familiar pop and crunching action) on the lateral side of the knee. I think I now understand what's causing this problem. From the beginning, the lateral side of my knee has held more swelling than the medial and, consequently, more scar tissue has developed in that region. When bending my leg there are restrictions to movement on the lateral side of the knee that aren't present on the medial side. I believe the medial side is then getting compressed as it continues to move while the lateral side is blocked. As the swelling continues to decrease and the scar tissue breaks apart, this problem should take care of itself. In addition to the regular home routine, I do lots of heel slides (50-60 holding for 10-20 seconds at the top) and no-weight prone curls to accelerate the breakdown of scar tissue.
February 4 - physical therapy session #8Electrical stimulation is eliminated from the routine and assisted stretches (calf, hamstring, and quadricep) are added. I continue with lots of heel slides and prone leg curls in the home routine and the pain is diminishing. I can do unassisted prone leg curls with bearable pain for a few repetitions.
February 7 - physical therapy session #9Therapy proceeds as it had for the past few visits. A Total Gym machine allows me to work my calves with less than full body weight on the knee.
February 7 - first day at workI begin a part-time, temporary assignment that involves a 30-minute commute and remaining seated for about six hours. Being seated without elevating the leg brings on uncomfortable stiffness and some swelling. Unfortunately, there is no way around this. Simply standing and moving while on the crutches helps a good deal in terms of loosening things.
General Notes - Week SixThe toe-touching exercise is interesting. Many of the nerves in my foot have been inactive for some time now and my foot tingles when it comes in contact with anything solid. This makes me consider the problem another knee surgery patient had. In her case, she too had also been non weight-bearing for a considerable period and, soon after returning to weight-bearing status, developed a stress fracture in the foot. The tingling sensation is a clear sign that the muscles of the foot aren't ready to absorb full weight-bearing force. Returning to FWB is going to be a gradual process - both the foot and the quadriceps need work. I also continue to have the sharp pinching sensation when bending my leg.
My knee is re-assessed for the purpose of submitting a recommendation to the insurance company. This is necessary to continue treatment as my insurance company approves therapy in groups of twelve visits. Submitting a request now should guarantee that therapy continues uninterrupted. The reassessment shows that the swelling has decreased nearly a centimeter and that my flexion has increased to roughly 134°. I begin to work on resuming a normal gait pattern, still using both crutches. In addition, a Kin Com machine is used to monitor my hamstring and quadricep strength in eccentric and concentric contraction. My leg muscles in general are still shaky and the Kincom machine shows it clearly in the jagged graphs that depict the muscle contraction throughout the movements.
General Notes - Week SevenI continue to work but no more than seven hours a day. As it did on the first day, the knee swells and stiffens after just a few hours but begins to loosen up with just a little movement. I do mobility exercises in the morning before work (40-50 heel slides, quad sets, prone leg curls (5 sets of 20 repetitions, no additional weight), and seated leg extensions (5 sets of 20 repetitions, no weight)). Each day after work I go to the gym where I ride a stationary bike for 12 minutes, no resistance - this helps loosen the knee tremendously. I'm now able to handle going every day but I monitor things carefully to keep from overdoing it again like I did in week five. Every other day in the gym, I complete a minimal leg workout (flexion and extension on the multi-hip machine, seated abduction and adduction, some isometric work on the leg extension and prone leg curl machines). I do upper body work as I'm able but this consists mainly of machine and light dumbell work. At the end of each workout I ride the bike again, this time for 10 minutes. I end the workout with lots of mobility exercises (towel-assisted heel slides to increase range of motion) and stretches. After this second bike ride, the knee is really warmed-up and flexible. This is where I make most of my gains in terms of increasing flexion and overall flexibility. I do mobility exercises and ice the knee again just before going to sleep. All of the low-stress, high-repetition activity does wonders for breaking up the scar tissue. By the end of the week, the sharp pinching sensation is reduced to minor discomfort. Also, several times throughout the week I focus on placing more and more weight on my foot, using my crutches as brakes of course. Rocking motions, both forward-to-back and side-to-side are best and I can feel tingling deeper in my foot with increasing weight. Self massage of the foot helps too, I wish I'd done more of this earlier. By the end of the week the nerves of the foot are much more alive but I still experience occassional tingling, particularly in the morning.
The routine stays the same. I do notice improvement in the graphs generated from the Kincom machine. The contractions are stronger and more consistent. A good deal of this visit is geared toward walking more normally. I started today on both crutches but, by the end of this session, I'm walking OK with one and am able to take a few steps with no crutches. I still feel unstable so it will be at least a few more days before I'm free of any support. My quadriceps aren't yet as strong as I'd like them to be while walking.
February 17 - post-op visit #6My sixth post-op visit is postponed for one week.
February 18 - physical therapy session #12The routine is no different than that of the 16th but I do spend a little more time with the therapist correcting my gait and re-thinking the mechanics of walking.
February 20 - AccidentWhile in the gym I trip and fall with my weight coming down solely on my left (where the ACI was performed) knee. Luckily, I'm near a wall so the fall is interrupted and my knee doesn't fully buckle. I don't experience any sharp pain but, of course, this is unsettling. There is some swelling in the evening but not a great deal more than before the accident.
General Notes - Week Eight
I go to the gym daily now even if it's only to ride the stationary bike and stretch. I'm working my upper body as much as I can using machines and dumbells. My gym leg routine, which I do every other day, is as follows:
In addition to the above, I do mobility exercises in the morning and evening before bedtime. There don't seem to be any adhesions left in the knee but it is still swollen with lots of fluid. Once warmed up, the knee moves quite easily but there is too much fluid and this makes flexion and extension difficult during the extreme portions of mobility exercises.
The routine stays the same. I seemed to have strained the vastus medialis oblique during one of my visits to the gym over the weekend. As a result, I'm unable to do some exercises but complete most of the routine. As my sixth post-op visit was postponed until tomorrow, my therapist performs another assessment of my knee and finds that the swelling has increased since the last assessment. Apparently, the swelling is costing me a few degrees flexion as I'm down to 128°.
February 24 - post-op visit #7My surgeon notes that the swelling is not unusual at this stage but agrees that it is probably inhibiting rehabilitation progress. He decides to aspirate the knee and withdraws 60 cc of fluid. The fluid is a bit bloody but not terribly so and my surgeon doesn't seem too alarmed. I'm instructed to stay away from the gym this evening and ice the knee. I cancel tomorrow's therapy session as well.
General Notes - Week NineI stay fairly inactive from Thursday through Sunday performing only mobility exercises followed by icing. On the Friday after the knee is aspirated the swelling is still substantial, I'm not sure I notice much difference from the day before. However, by Saturday the swelling is reduced considerably. I think that Friday's swelling was in part due to the trauma of having the needle in the knee and it simply took a few days to recover. On Monday I begin driving my manual transmission vehicle again and it's a bit uncomfortable but not too much so. I return to the gym and continue with the leg routine listed earlier with a few changes focused more on regaining strength: a bit more resistance on the bike and slight increases in the weights used in the exercises. I also decrease the number of repetitions to 15 as opposed to 25.
The knee feels much better than a week ago. I'm now stronger and have greater range of motion with less effort. My routine in therapy stays much the same but I'm now able to perform squatting movements, at an angle, on the Total Gym machine. In addition, I'm allowed to perform calf raises on a lying leg press machine. I also begin exercises to regain proprioception, starting with simply standing on the injured leg with my eyes closed (four sets of fifteen seconds each). This is much harder than it sounds.
March 3 - physical therapy session #14The knee looks even better today and is more flexible. My therapy routine stays the same with the exception that I now stand on a trampoline when performing the single-leg balancing exercise. My knee is feeling pretty flexible when I get home and I'm even able to take a few stairs without using a handrail or anything else to assist.
General Notes - Week TenMy range of motion has increased significantly and it requires less effort to get to the upper limits of flexion. I do continue to have a noticeable limp and stairs still require a handrail but things have certainly improved since the knee was drained. Therapy has grown sufficiently difficult and I no longer feel the need to supplement it with my own leg workouts. I do ride the stationary bike each day and stretch but that's it for the leg on days when I'm away from the gym.
There are a few exercise changes in the routine and additional weight/lower repetition substutions. Instead of seated hamstring curls, the Kincom machine is used to exercise the hamstrings. This machine reveals weaknesses at the extremes of my range of motion.
At this point in therapy, my routine is structured as shown below:
Today's workout is the most taxing yet but my leg appears no worse for the effort.
March 10 - physical therapy session #16Not much change from the March 8 session.
March 12 - massage therapy session #1In an attempt to eliminate the last bit of swelling, I see a massage therapist. She works on the knee for most of the session using a homeopathic anti-inflammatory ointment - Traumeel. After the session, there is some noticeable reduction in the swelling but, more importantly, it feels better and I'm able to walk down a flight of steps with little limping. Unfortunately I'm on my feet for most of the remainder of the day which irritates the knee. I will probably try this again. I buy some of the Traumeel for use at home.
The routine is modified slightly as shown below with additions and changes highlighted:
No changes from the previous session.
General Notes - Week TwelveI still have swelling and it's still a bit warm to the touch, but I can now move up and down steps with greater ease although not yet smoothly. I continue to apply the Traumeel.
Much the same as in the past few sessions with the following addition: a game of catch is introduced - balancing on the injured leg, while on a trampoline, I toss a weighted ball back-and-forth with my therapist.
March 27 - physical therapy session #20The routine is the same as before with the following exception: stationary bike replaced by Precor elliptical trainer - 10 minutes.
General Notes - Week ThirteenAs I've been riding the stationary bike, I've found that low tension, high revolutions-per-minute training really seems to loosen things up. My therapist doesn't seem to think that this will cause any problems.
The exercise routine is the same as my last session. I have a follow-up visit with my surgeon tomorrow so a reassessment is performed. Swelling is down by 1.5 cm since the last measurement but it is still noticeable. My therapist and I agree that I'm probably able to go on my own but we'll wait until I've spoken with my surgeon before making any final decisions.
March 32 - massage therapy session #2I see the massage therapist again with the goal of reducing swelling and removing tension I've developed in my upper back and neck. She also performs some deep-tissue manipulations on my hamstrings to increase flexibility. As was the case in the previous session, I find it easier to handle steps afterward.
March 31 - post-op visit #7My surgeon doesn't seem too alarmed over the swelling. He recently attended a conference and several surgeons from Europe (where ACI has been performed for a longer period) stated that it now appears as if it may take as long as two years before the cultured chondrocytes fully mature. As a consequence of this fact and the rather invasive nature of ACI, swelling as long as nine months post-op is not seen as terribly unusual. Nonetheless, my surgeon tells me that if I have the same amount of swelling next month, he will probably aspirate again. He also believes that I'm ready to proceed on my own in terms of rehabilitation. I also ask my surgeon about the fast biking and he seems to think that this is OK as long as I use lower resistance.
April 2 - physical therapy session #22My routine is much the same as before with the addition of a few lateral motion drills involving a theraband. I discuss the rehabilitation protocol with my therapist. I have no real questions about how to proceed from here so I'm discharged from formal therapy. My therapist and her staff were great throughout all of this and I'm very grateful. A good therapist and team make a big difference.
I break up my routine so that I do quadricep and hamstring exercises on different days, but I perform weightlifting movements with each muscle group only once per week. However, I do continue stationary biking every day and have increased the intensity. I now ride for no less than 25 minutes per day and I pedal rapidly at low resistance. In terms of day-to-day activities, I am still unable to take stairs and hills without a limp.
No big changes relative to last week. The routine is the same and I still have the same difficulties with stairs and inclines.
The weightlifting routine is the same as the past two weeks but I've now added two rounds of stationary biking each day. This doesn't make things any better or worse so I continue. I'm aware that I don't use the involved leg nearly as much as the good leg when biking and I begin to focus strongly on trying to "even out" this exercise. I still use low resistance and try to maintain fast pedaling throughout the exercise. I rake and mow the yard.
There is still a bit of swelling but otherwise no pain. Nonetheless, my surgeon feels it best to remove the existing fluid from my knee. Roughly 25 cc of a slightly orange fluid are removed with relative ease. My knee is noticeably more mobile after this. Otherwise, things appear to be in good shape from my surgeon's perspective.
For the early part of the week, I'm sick with a virus and am not very active. The knee doesn't seem to change much during these couple of days before my eighth post-op visit.
My workouts remain the same. I ride the bike in the morning and, in the evening, I ride the bike as well as lift weights. I do substitute treadmill exercises for the bike in some of my evening workouts. While on the treadmill, I walk straight, perform side-to-side stepping, and backward walking. I do quadricep and hamstring exercises on different days and work each of these body parts twice per week. I also try to exercise calves three times per week. The biggest breakthrough I notice is that I'm able to perform leg extensions much more smoothly now, even though I'm using very little resistance (20 pounds).
For better or worse, I stop wearing my brace. I have more difficulty contracting my quadriceps while in the brace and I think I'll get tone in these muscles more quickly by doing my day-to-day activities without the brace. It's a bit risky I suppose but I think it's not likely to be a problem as long as I'm careful.
I'm now adding the Precor elliptical trainer to my workouts with most of my effort directed at keeping the movement natural (i.e., using my left leg as much as my right).
Stairs are still a bit clumsy. I think this is mainly a function of my not-yet-toned and slow-firing quadriceps. It seems that as they get stronger, the stairs become less of a challenge. This makes perfect sense but before I had thought most of the problem was a result of my knee as opposed to my quadriceps. I now think that my weakened quadriceps have been putting too much of the force on the knee.
I've discovered that the Precor elliptical trainer is irritating my knee. Even though it's relatively non-impact, compared to stair-climbing machines, I think this exercise is placing too much compression on the cartilage implantation site. I stop using this machine.
I am still able to exercise quite regularly though. Three or four days of the week I go to the gym in the morning for stationary biking and stretching and am able to go back in the evening for more biking and weight-training.
Stubborn I suppose, but as I felt particularly good one day, I decided to try using the Precor device once more. Again, this proves to be a bad decision. My knee swells and becomes weaker, just in time for my next visit to the surgeon.
May 25 - post-op visit #9My surgeon notes that the swellling is greater than at my last visit and I explain that I've been more aggressive with my activities. He decides to not aspirate the knee and instead gives me a prescription for Relafen, a nonsteroidal anti-inflammatory medication.
A few days after taking the Relafen, I notice a significant decrease in swelling. My knee has not felt this good since the surgery. Stairs have become much easier and I can almost handle going up and down stairs with a smooth gait. I don't attribute this all to Relafen although it appears to have helped in the swelling. My knee has looked this good recently (in terms of swelling) but I think I now have the quadricep strength needed to handle more easily things like steps and inclines.
With my new, noticeable improvements, I immediately get overconfident and attempt more demanding weight-training movements, like pressing exercises. What a mistake, my knee promptly responds with increased swelling and feels weaker almost like it did before the last aspiration (April 27). I increase the dosage of Relafen (1000 mg to 1500 mg, daily) and decrease my activity, taking Sunday off altogether. I resume working out on Monday and put myself through a demanding leg routine. Oddly enough, my leg responds well to this and it feels like there's some scar tissue breaking up which provides some feeling of relief.
I continue to have considerable swelling but it's not warm (which would indicate blood in the fluid, and some sort of damage). It does restrict, to some degree, the ease with which I move my leg, but overall it's not a big problem. I'm now working out twice a day with biking (30 minutes) and stretching in the morning and weight-training, biking (20 minutes), treadmill (10 minutes), and stretching in the evening. As the week continues, I become a bit more aggressive, adding weight to the leg exercises I'm doing and raising the treadmill speed and incline. On some days I'm spending 20 minutes on the treadmill as follows:
On Friday I notice what appears to be a moveable knot on the medial side of my left knee, right along the joint line. This sends me spiraling into a mode of uncertainty and fear, thinking that I may have dislodged the now semi-mature implanted cartilage. Over the weekend, this doesn't improve, nor does it degenerate, but I'm thinking I've really done some harm. Thinking the worst, I begin researching total knee replacements. My tenth post-op visit to the surgeon is scheduled for June 14, but with the knot on the side of my knee, I phone the surgeon's office and they are able to move my appointment to today, Monday, June 11.
June 11 - post-op visit #10My surgeon informs me that the knot I'm feeling is nothing other than a slightly inflamed tendon. The relief I feel is indescribable. There is still a fair amount of "clunking" when he manipulates my knee through rotational movements. He assures me that this is primarily scar tissue. He seems pleased overall, but does have some minor concern over the swelling although it's not entirely unexpected at this stage. He tells me that if this same level of swelling exists at my next visit, he will aspirate. Otherwise, I'm instructed to ice and continue with the Relafen. Admittedly, I've neglected icing for most of the past few weeks.
During the week I notice a growing numbness in my right arm and something that feels like the beginnings of a strained muscle in my right calf. These are the latest symptoms in a known problem. Through all of my surgeries, I've developed a tendency to sit and stand with most of my weight directed toward my right side. This has caused cramping in my upper back and neck and now the numbness and overworked right leg muscles. I also notice that it is rather hard to stand straight with my weight evenly distributed between both legs. I see a massage therapist for the numbness and cramping and, while that provides temporary relief, the problem reappears the next day. All through the week I pay particularly close attention to my alignment during stretching movements and it becomes apparent to me that I still do not extend my left leg as much as my right when standing. This leads to something of a rotation in my hips with a slight bend in my left knee. This is all very subtle and I'm sure unnoticeable to anyone else but I certainly see and feel it. Throughout the week I focus on stretching my left leg, mainly the hamstring and iliotibial band, in an effort to restore more balance. This is also going to require a conscious effort to sit straight and focus on better posture.
I should mention that the numbness in my right arm, mentioned in last week's entry, is compounded by what was probably a torn rotator cuff injury I had a few years ago. This rotator cuff problem has been with me for some time but it's manageable and, with any luck, I hopefully won't be developing another joint injury web site in the future.
Although the tendon inflammation still exists, I feel good enough to try bicycling for real. I take a fifteen-mile ride on Saturday and I'm no worse for the wear afterward. I continue with weight-training and lots of stretching. In one particularly long stretching event, I feel my hamstring tendons "open" up.
Even though the stretching is helping to correct my posture and my gait seems to be more even, I'm still feeling the numbness. I decide to see a chiropractor and he notices a positional problem with my right shoulder blade; I can feel it and am all-but-certain that this is the result of the poor posture I've developed in my post-op periods.
I continue with the biking and weight-training and finish a 20-mile, as well as a 34-mile, ride. I also increase the amount of weight I use in my quadricep training and I begin to perform lying leg presses (using very light weight). The tendon inflammation is still with me and it's causing some trouble with my gait, but nothing too terrible.
The chiropractor treatments are helping with the numbness. I continue with my regular routine as far as weight-training is concerned, with three, two-workout days. On Saturday and Sunday, I take two 25-mile bike rides and the only trouble I experience is quadricep soreness. I suspect that some of the trouble may be attributable to a tight iliotibial band and so I increase stretching in that area. As a result of my efforts at better posture, the stretching, or time (most likely a combination of the three), the tendon doesn't seem as inflamed on Monday as it has been.
July 10 - post-op visit #11My surgeon notes some swelling and says it's unusual but not alarming since I have full flexion/extension and no pain. He said that one hypothesis on why some people experience this swelling is that it's a reaction to the sutures used to hold the periosteal patch in place. The swelling may be present for as long as 1 - 1.5 years following surgery. As far as the iliotibial band tendon problem, my surgeon recommends continued icing and application of some sort of cream.
I begin using DMSO to treat the inflamed tendon.
First, apologies for the long delay in updating this site. I had to move, which became complicated resulting in putting things into storage for over a month, and I didn't have access to my HTML files.
I continued to see the chiropractor through the end of July and the numbness I had been feeling in my arm and hand disappeared. I've seen chiropractor's on three different occassions now, and this was easily the most successful and satisfying series of treatments. If you're looking for a chiropractor in the Arlington, VA area, I can recommend:
Drs. Kevin and Kristine Maggs
Arlington Neck & Back Center
6015-A Wilson Blvd.
Arlington, VA 22205
(703) 536-5900
As far as the DMSO is concerned, I stopped using it soon after I began. I simply couldn't find much guidance on how it should be applied to any mammal other than a horse.
July was a tough month for the knee. I painted the interior of a house and moved. There were many 16-hour days of standing, lifting, and carrying heavy objects. This left my knee and leg sore, but I quickly recovered after the painting and moving was over. I continued weight-training and biking during this period as well and it seemed to relieve some of the pain and stiffness resulting from the constant standing.
Aside from moving my self again at the beginning of September, the period from August to October was pretty uneventful. I continued weight-training and biking. The strength, as well as tone, in my quadriceps continued to improve. In October, I began riding my road bike on Skyline Drive, in Shenandoah National Park. One of the 20-mile routes I found involved a roughly five-mile uphill portion through an elevation gain of 1000 feet. The ride is more of a cardiovascular strain than it is a challenge for my knee. I've added some more aggressive exercises to my weight-lifting routine such as front squats and stiff-legged deadlifts.
I still feel discomfort in a deep squatting position and I still tend to lean more toward my right, but I still believe that things are improving. I haven't yet tried backpacking, but probably will soon.
October 5 - post-op visit #12It's much the same story as last time. My surgeon notes the same swelling and says it's unusual but not alarming since I have full flexion/extension and no pain. He also said that I'm pushing my knee above-average and that is likely contributing to the swelling, in addition to the hypothesis that it's a reaction to the sutures used to hold the periosteal patch in place. He reiterates that the swelling may be present for as long as 1 - 1.5 years following surgery.
I ask about the pain and discomfort I experience in a deep squatting. He said this is expected for the following reasons: I'm still recovering; I have some wearing of the articular cartilage both behind the patella and in the trochlear notch; and regardless of the health of the knee, the deep squatting position is extremely taxing for the joint as it results in a force of over eight times one's body weight.
Over the past month, I took two hikes, both with fairly steep ascents and descents. On one of the hikes, I slightly twist my knee and I feel something strange. The sensation isn't really painful, but not normal either. My knee swells a bit more than usual and I feel a little pain whenever the knee bends while bearing weight. I lay off exercise for a few days and the swelling decreases.
The swelling continues to decrease and my knee now looks better than it has since the surgery. It feels like a more natural motion is coming back to simple, day-to-day activities (e.g., rising out of a seated position). Certain weightlifting exercises, like front squats and standing calf raises, still irritate my knee and sometimes lead to swelling (which usually lasts for a day or two). I do seem to be improving though.
I haven't yet tried hiking again, and I wouldn't be comfortable with any activity that demands quick, lateral motion. I'll go hiking soon and if it causes any trouble, I may try trekking poles. My surgeon told me during the last visit that it's now time to start finding boundaries for my knee. In addition, I'm still healing, so this is a time of trial-and-error.
I've hiked several times since my last diary entry with no big problems, but without complete confidence. The past six weeks have seen little activity, mainly due to a bout with bronchitis. I have noticed a range of sensations in weight-training though, from a squishy feeling under loaded compression to greater stability and confidence in deep squatting positions. Since these are conflicting pieces of data, I'm not sure what to make of my current situation. I'm still encouraged though and have felt more positive changes recently.
I still plan to soon test my knee while hiking, given that I recover fully from the respiratory infection.
October 5, 2000 - post-op visit #13My surgeon offers another explanation as to why my knee may retain swelling, but not be painful. Repeated trauma to the knee damages the synovium, the membrane that encapsulates the knee joint. This, in turn, limits the ability of the synovium to absorb any swelling that naturally occurs in the knee. Any time a knee undergoes stress, such as in demanding exercise, the joint responds with an increase in synovial fluid output. A normal, healthy synovium absorbs this fluid rather quickly, but a damaged synovium isn't as efficient. My surgeon doesn't seem alarmed by this, as long as there is no pain.
We still plan to have a follow-up MRI in June, the 18-month mark after my surgery. I have no further scheduled appointments with my surgeon until then.
I took a few photos of my knee that might be of interest. The scars are the result of five surgeries. The longest two, down the front center of my knee are what you would expect following an ACI. The top scar is left by the incision used to implant the chondrocytes while the bottom scar corresponds to the incision used for removing the tibial periosteum. Since I've had three surgeries that all involved incisions along the axis of the patellar tendon, my scarring in that area looks wider than it might if only one surgery had been performed.


I'm still testing my knee. Since the last writing, I've been on hikes of 4, 7, and 10 miles and have been pretty active in general. After the hikes, all of which were over rough terrain, my knee was sore but I recovered within day or two.
I still have an irregular gait that I notice and feel but hardly anyone else sees it. The irregularity is subtle and involves my calf muscles. My calf muscles don't respond as quickly as in my good leg and have gotten "lazy" which I'm sure is translating into more shock to my damaged knee. This has been an issue for some time, becoming most noticeable after my second ACL reconstruction. I'm trying to walk more consciously, ensuring that my calves are equally involved. I'm also going to focus more on my calves in the weight room.
Note to those rehabilitating following a knee surgery: put considerable focus on your calves, not necessarily in the form of heavy resistance but definitely using many repetitions. Calf muscles are characterized by high-density fibers and require many repetitions before responding and conditioning.
There's nothing radically different from my last visit. My surgeon explains to me once again how it's difficult to predict and analyze the conditions of a knee on which has experienced multiple trauma. However, he notes that the knee looks good, all things considered, and that my muscle tone seems OK. We elect not to have the follow-up MRI as it would be yet another expense and, since I'm not complaining, and unnecesary cost at that. I agree and leave the office with no plans to return, unless there's a compelling reason to do so.